Paper
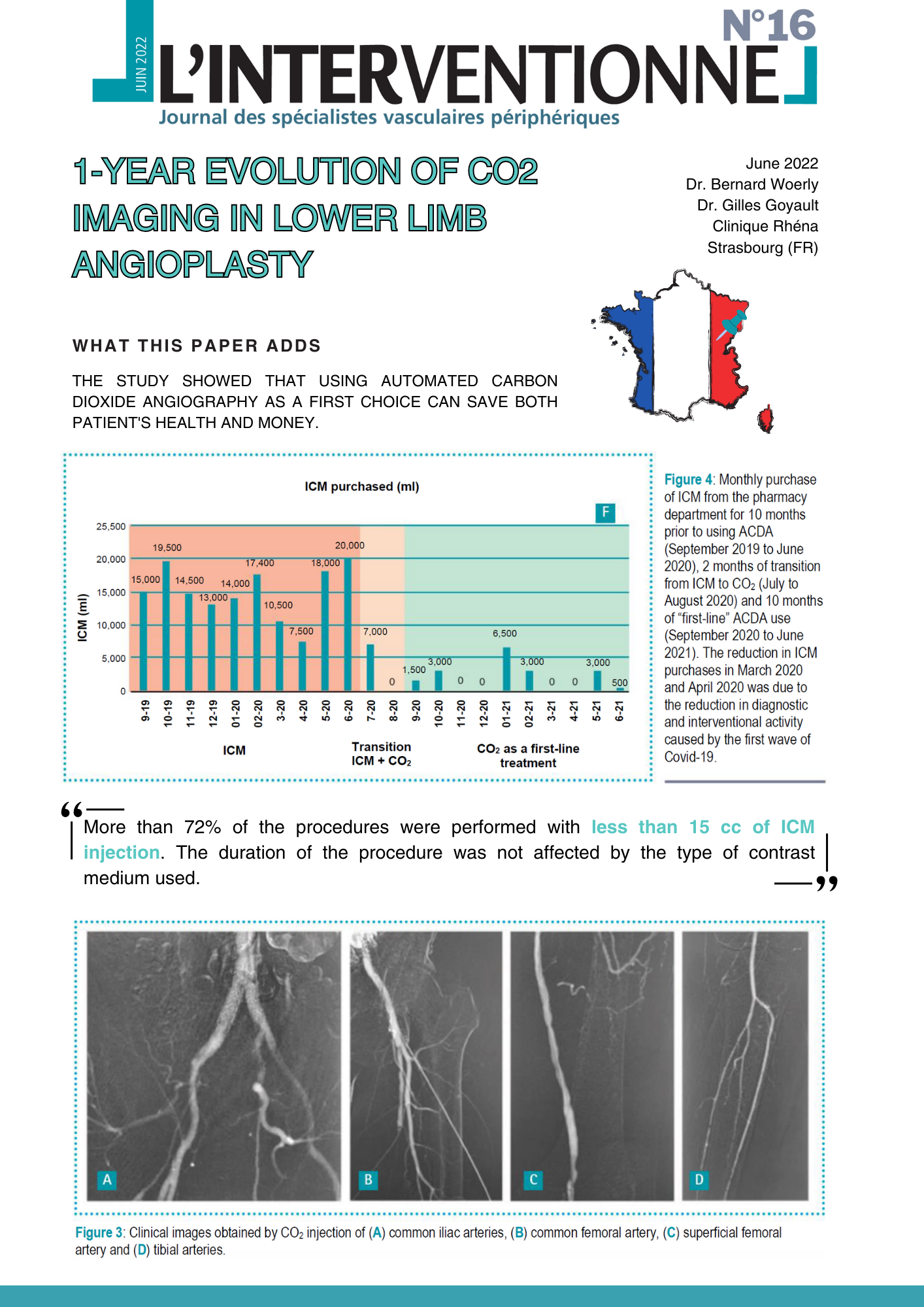
1-year evolution of CO2 imaging in lower limb angioplasty
INTRODUCTION: Manual or semi-manual CO2 injection systems do not allow for repeatability of the...
Paper
Carbon Dioxide As a Standard of Care for Zero Contrast Interventions
Background: Traditional contrast media containing iodine remain the gold standard for vessel...
Paper
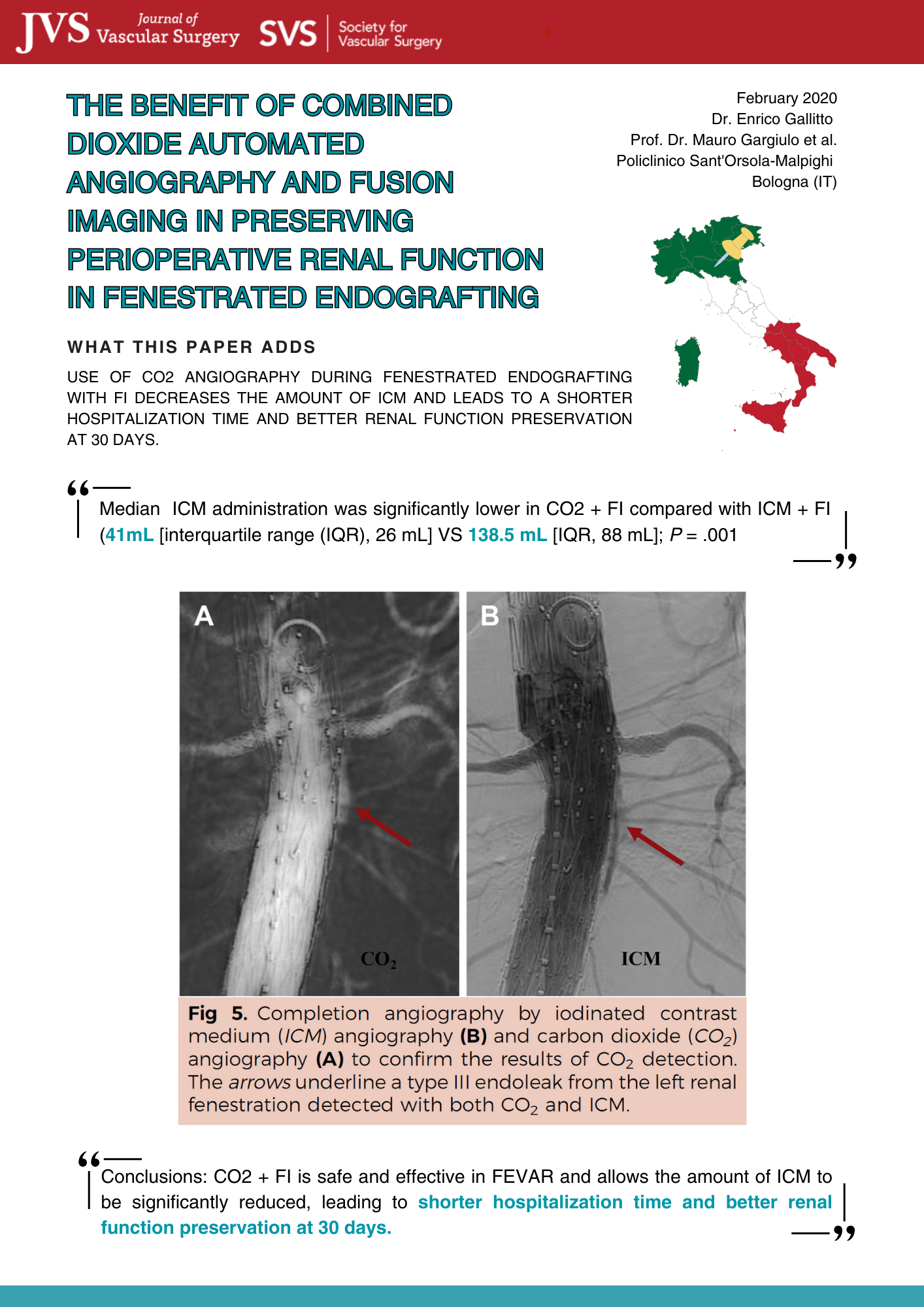
The benefit of carbon dioxide automated angiography in FEVAR
Background: Contrast-induced nephropathy is a possible adverse event in fenestrated endovascular...
Paper
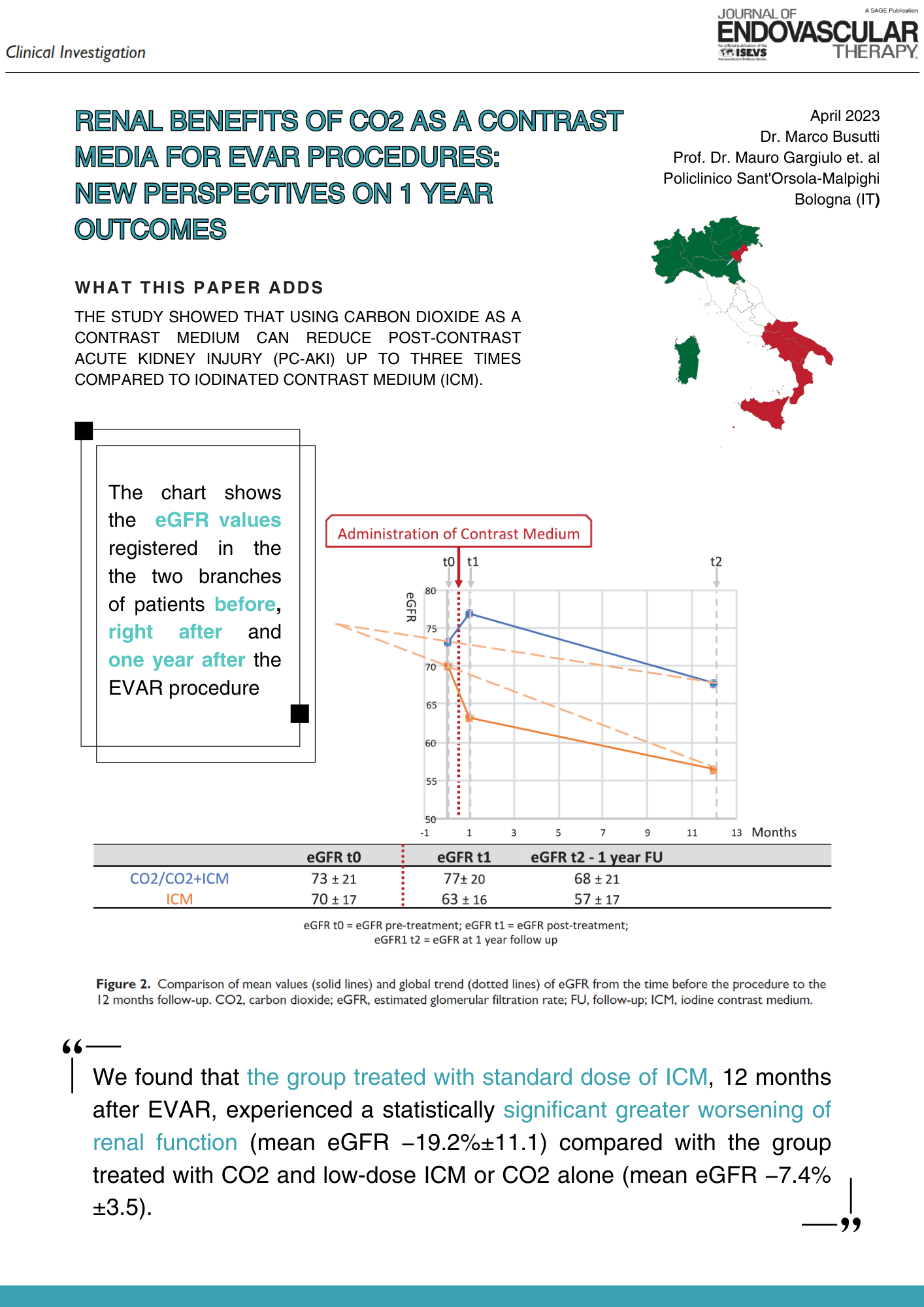
Renal Benefits of CO2 as a Contrast Media for EVAR Procedures
Background and Objectives: Endovascular aneurism repair (EVAR) is a minimally invasive alternative...
Paper
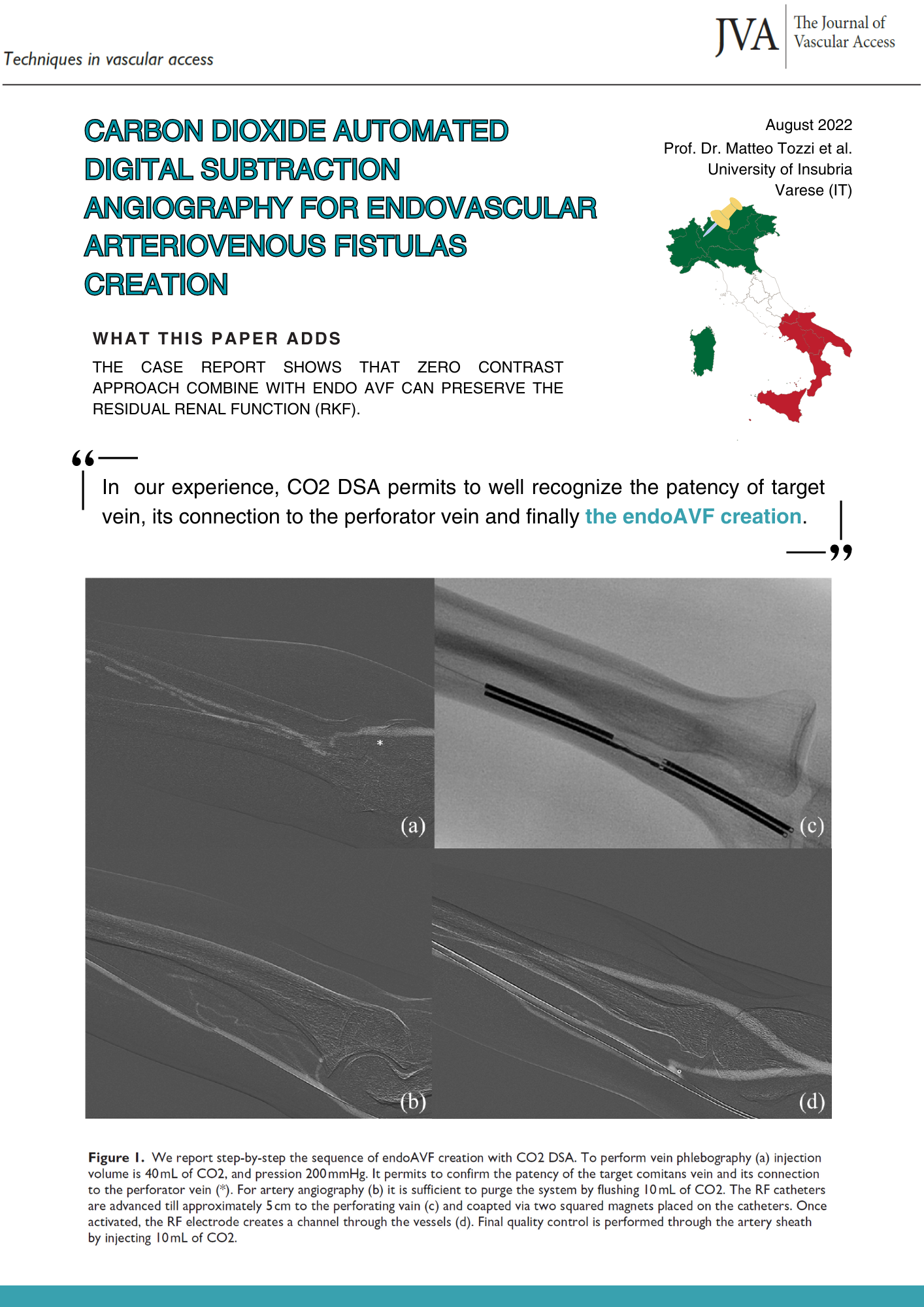
CO2 automated digital subtraction angiography for endoAVF creation
Recent literature shows how residual renal function (RKF), defined as the urinary clearance of urea...
Paper
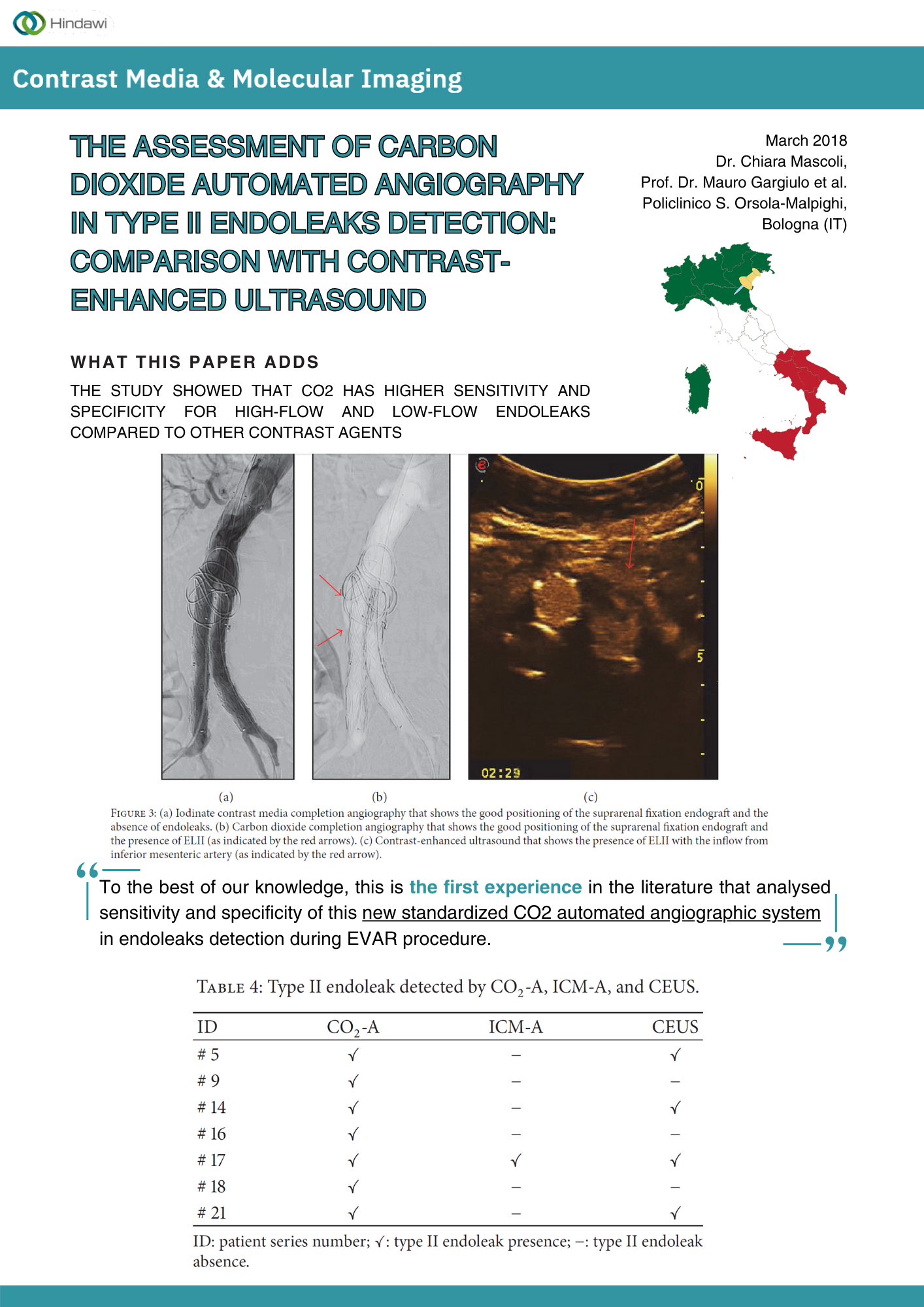
The Assessment of CO2 Automated Angiography in Type II Endoleaks Detection
Introduction: Iodinated contrast media completion angiography (ICM-A) may underestimate the...
Paper
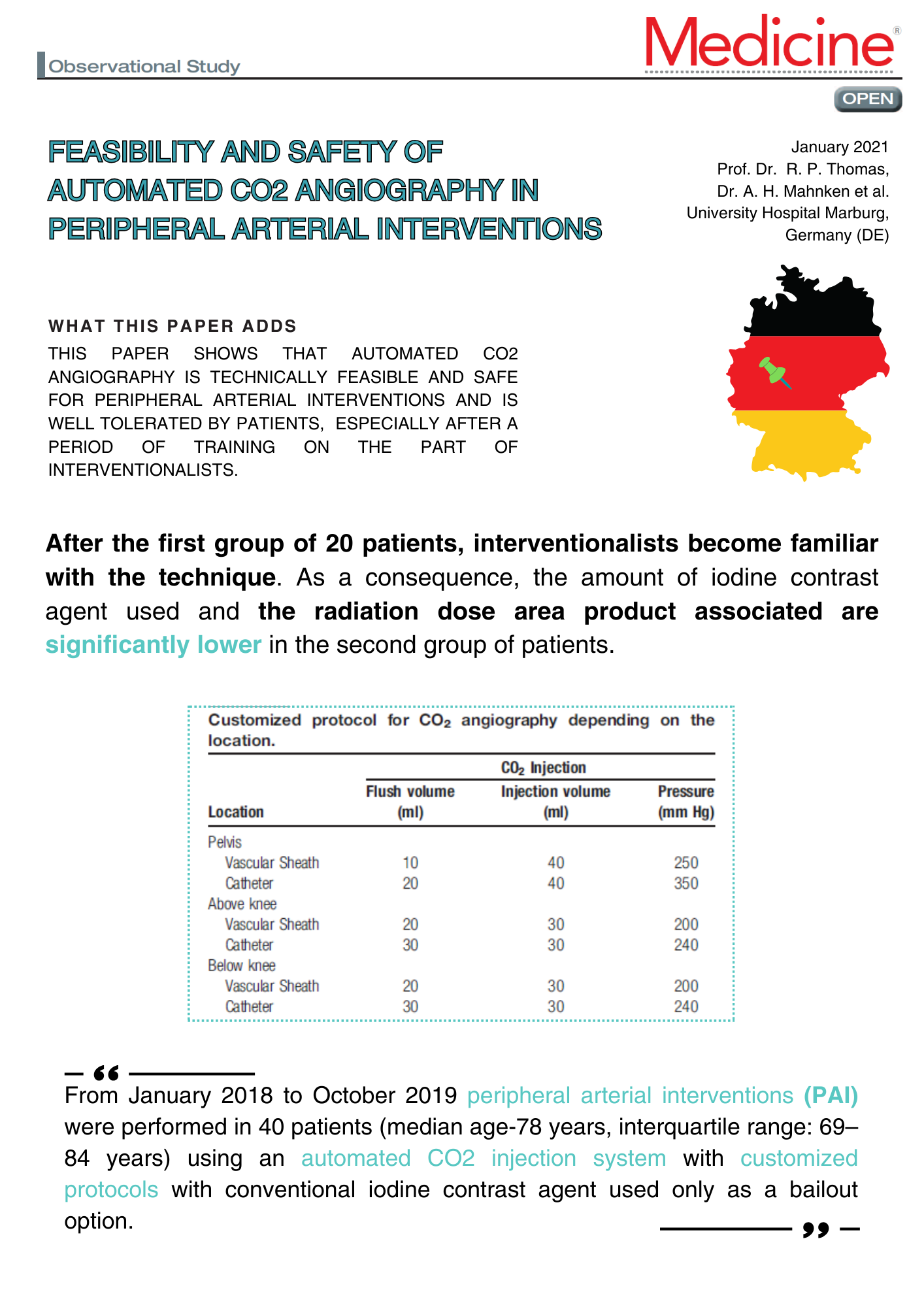
Feasibility of CO2 angiography in peripheral arterial interventions
Carbon dioxide (CO2) gas is an established alternative to iodine contrast during angiography in...
Paper
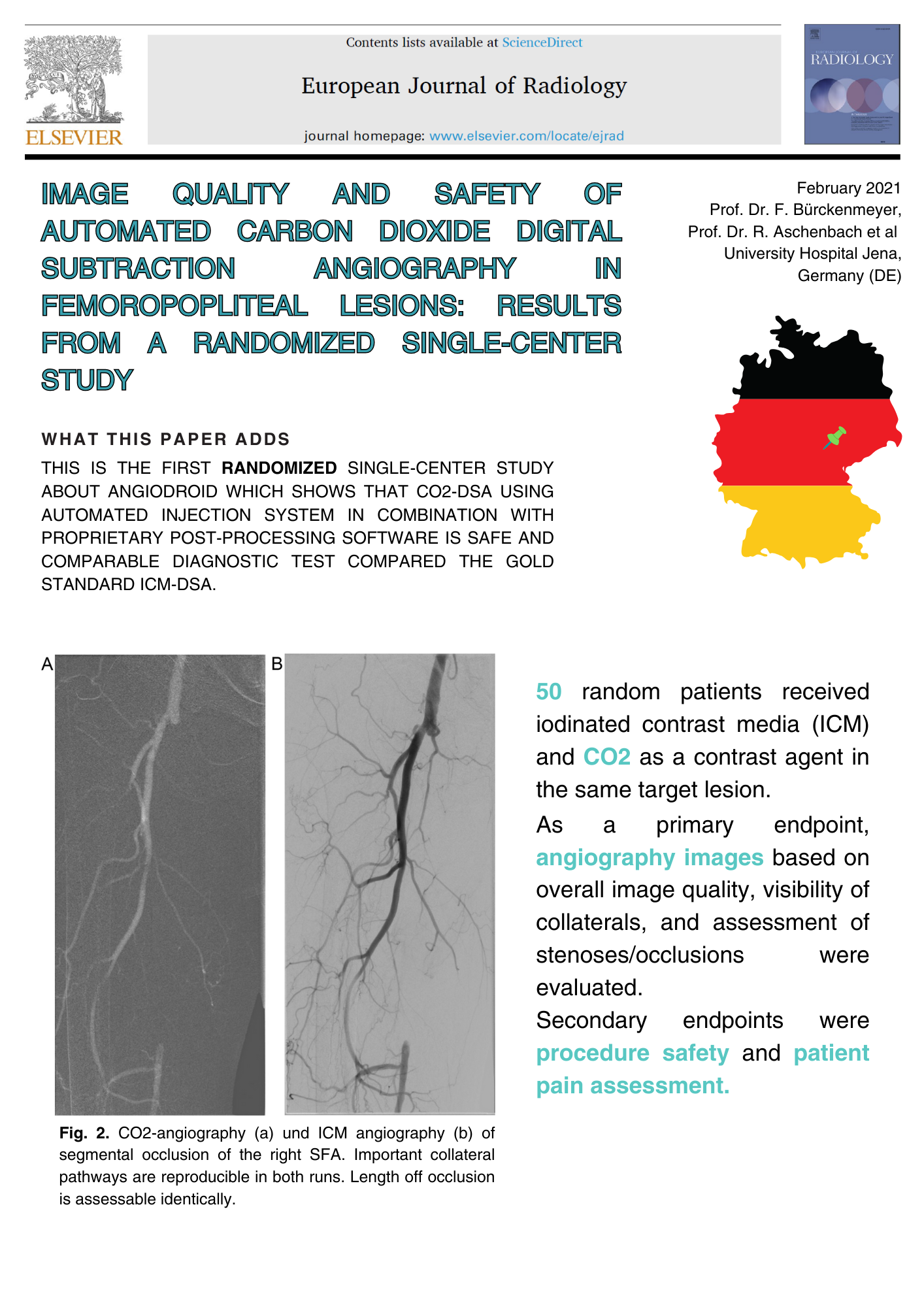
Image quality and safety of ACDA in lower limbs
Purpose: To evaluate the image quality and the safety of automated carbon dioxide (CO2) digital...